Mastering ADHD: A Comprehensive Guide to Understanding and Thriving with Attention Deficit Hyperactivity Disorder

Finding the right diet for a child with ADHD can be tough, especially with all the different advice out there. It’s important to know which foods can help improve focus and behavior, and which ones might make ADHD symptoms worse.
In this article, I’m going to share the best diet for kids with ADHD in 2024. We’ll cover foods that are good for brain health and those to avoid, making it easier for you to make the right food choices for your child’s needs.
What is ADHD?
ADHD, or attention-deficit/hyperactivity disorder, is a neurodevelopmental disorder that affects both children and adults. It is characterized by persistent patterns of inattention, hyperactivity, distractibility, poor working memory, and impulsivity that can significantly impact daily functioning and quality of life.
Individuals with ADHD may have difficulty staying focused, paying attention to details, organizing tasks, and maintaining sustained mental effort. They may also exhibit excessive physical activity, restlessness, and fidgeting.
ADHD Statistics¹
According to a study done by the Center for Disease Control and Prevention in 2016, over 6 million children in the United States (9.4 percent) have been diagnosed with ADHD.² ADHD is one of the most common childhood neurodevelopmental disorders, according to the DSM-5.³ Although specific statistics may vary, it is estimated that approximately 5 percent of children worldwide are affected by ADHD.⁴
ADHD Types
There are 3 subtypes of ADHD: Hyperactive-Impulsive type, Inattentive type, and Combined type. It is important to understand these different types as it can help inform appropriate diagnosis and treatment strategies tailored to address the specific challenges and symptoms experienced by individuals with ADHD.
ADHD Hyperactive-Impulsive Type
ADHD Hyperactive-Impulsive type is one of the three subtypes of attention-deficit/hyperactivity disorder (ADHD). Individuals with this subtype primarily exhibit symptoms of hyperactivity and impulsivity, while their ability to maintain attention may be less affected. People with ADHD Hyperactive Impulsive type often have difficulty sitting still, constantly feel the need to move, and may engage in impulsive behaviors without considering the consequences. They may interrupt others frequently, struggle with impulse control, and find it challenging to wait their turn. These symptoms can significantly impact daily functioning and social interactions, making it important to provide appropriate support and interventions tailored to their specific needs.
ADHD Inattentive Type
ADHD Inattentive type, also known as ADHD Predominantly Inattentive type, is one of the subtypes of attention-deficit/hyperactivity disorder (ADHD). Individuals with this subtype primarily experience difficulties with attention and focus, while hyperactivity and impulsivity may be less pronounced. People with ADHD Inattentive type often struggle to sustain attention, become easily distracted, and have difficulty organizing tasks or following through on instructions. They may appear forgetful, have trouble staying organized, and often seem to daydream or be lost in their own thoughts. These symptoms can significantly impact academic performance, work productivity, and interpersonal relationships. It is essential to recognize and address the specific challenges associated with ADHD Inattentive type to provide appropriate support and interventions for individuals affected by this subtype.
ADHD Combined Type
ADHD Combined type is a subtype of attention-deficit/hyperactivity disorder (ADHD) that encompasses a combination of symptoms related to inattention, hyperactivity, and impulsivity.
Individuals with ADHD Combined type experience difficulties in multiple areas of functioning. They may struggle to sustain attention, exhibit hyperactive and impulsive behaviors, and have difficulty controlling their impulses. These individuals may often be fidgety, talk excessively, interrupt others, and have trouble waiting their turn.
The symptoms of ADHD Combined type can significantly impact various aspects of daily life, including academic performance, relationships, and overall functioning.
It is important to provide comprehensive support and interventions tailored to address both the inattentive and hyperactive/impulsive symptoms to help individuals with ADHD Combined type thrive and reach their full potential.
ADHD Symptoms in Kids
Children with ADHD may exhibit a range of symptoms that can impact their daily functioning and overall well-being. These symptoms can be categorized into two main domains: inattention and hyperactivity/impulsivity.
It’s important to note that the severity and combination of symptoms can vary among children with ADHD.
Recognizing and understanding these symptoms is crucial for early identification, appropriate diagnosis, and implementing effective strategies to support children with ADHD in their academic, social, and emotional development.
Hyperactivity and Impulsivity ADHD Symptoms
Hyperactivity and impulsivity symptoms involve excessive fidgeting, difficulty staying seated, talking excessively, interrupting others, and acting on impulse without considering the consequences.
Inattentive ADHD Symptoms
Inattentive symptoms include difficulty sustaining attention, being easily distracted, making careless mistakes, forgetfulness, and having trouble organizing tasks or activities.
ADHD in Girls Versus ADHD in Boys
ADHD can present differently in girls compared to boys, often leading to underdiagnosis or misdiagnosis in girls. While boys with ADHD typically display more hyperactive and impulsive behaviors, girls tend to exhibit more internalizing symptoms and difficulties with attention. Girls with ADHD may be less disruptive in the classroom and may be overlooked or perceived as daydreamers or shy. They often internalize their struggles, leading to feelings of anxiety, low self-esteem, and perfectionism. Girls with ADHD may also demonstrate more social withdrawal and be more prone to self-harm or eating disorders. Additionally, they may be better at masking their symptoms by using coping mechanisms such as hyperfocus or people-pleasing. These differences in ADHD presentation highlight the importance of recognizing and understanding the unique challenges faced by girls with ADHD to ensure accurate diagnosis and appropriate support.
ADHD Diagnosis or Misdiagnosis
How is ADHD Diagnosed?⁵
ADHD diagnosis involves a comprehensive evaluation process that considers various factors to determine if an individual meets the criteria for the disorder. Typically, diagnosis b
egins with gathering information from multiple sources, including parents, teachers, and other relevant individuals, who provide insights into the individual’s behavior and symptoms across different settings.
The diagnostic process involves assessing the presence and severity of core symptoms of inattention, hyperactivity, and impulsivity, as outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
Other factors, such as the duration and onset of symptoms, their impact on daily functioning, and the exclusion of alternative explanations for the symptoms, are also considered.
The evaluation may involve psychological assessments, behavioral observations, rating scales, and interviews conducted by healthcare professionals specializing in ADHD.
It is crucial to rule out any underlying medical conditions or psychological factors that may contribute to the symptoms. By gathering comprehensive information and utilizing standardized diagnostic criteria, healthcare professionals can accurately diagnose ADHD and develop an appropriate treatment plan tailored to the individual’s specific needs. A thorough and accurate diagnosis is the foundation for effective management and support for individuals with ADHD.
Is ADHD Misdiagnosed?
The issue of ADHD misdiagnosis has been a subject of debate and concern within the medical and mental health communities. While ADHD is a legitimate and widely recognized neurodevelopmental disorder, there are instances where misdiagnosis can occur. Factors contributing to misdiagnosis include the complex nature of ADHD symptoms, which can overlap with other conditions, such as anxiety, depression, or learning disabilities. Additionally, the subjective interpretation of symptoms and reliance on reported behaviors from multiple sources can introduce potential biases and inaccuracies in diagnosis. The misdiagnosis of ADHD can lead to inappropriate treatments or interventions that may not address the underlying issues. It is crucial for healthcare professionals to conduct thorough assessments, consider a range of potential diagnoses, and utilize standardized diagnostic criteria to minimize the risk of misdiagnosis. Collaborative efforts involving multiple professionals, such as psychologists, psychiatrists, and educators, can provide a more comprehensive evaluation and improve the accuracy of diagnosis. Ongoing research and training initiatives focused on improving diagnostic practices can further help reduce the rate of misdiagnosis and ensure that individuals with ADHD receive appropriate support and interventions.
ADHD Causes
The exact causes of ADHD (Attention-Deficit/Hyperactivity Disorder) are not yet fully understood. However, research suggests that a combination of genetic, neurological, and environmental factors play a role in its development.
Genetics:
ADHD tends to run in families, indicating a genetic component. Certain genes involved in brain development, neurotransmitter regulation, and dopamine signaling have been implicated in ADHD. However, it’s important to note that having a family history of ADHD does not guarantee that a child will develop the disorder.
Neurological Factors:
Studies using brain imaging techniques have revealed differences in the structure and activity of certain brain regions involved in attention, impulse control, and executive functions in individuals with ADHD. These differences suggest that abnormalities in brain development and functioning may contribute to the symptoms of ADHD.
Environmental Factors:
Various environmental factors have been associated with an increased risk of developing ADHD. These include exposure to toxins during pregnancy (such as tobacco smoke or lead), premature birth, low birth weight, maternal substance abuse, and prenatal exposure to alcohol or certain medications. Additionally, factors like high levels of stress in the family, chaotic home environments, and inconsistent parenting practices may also contribute to the manifestation of ADHD symptoms.
It’s important to note that ADHD is a complex disorder with multifactorial causes, and each individual’s experience with ADHD may be unique. Ongoing research aims to further explore the interplay between genetic, neurological, and environmental factors to gain a better understanding of the underlying causes of ADHD.
Underlying stressors can certainly exacerbate ADHD symptoms, even if they are not the direct cause of the disorder.
Genetic expert and founder of The DNA Company, Kashif Khan, estimates that only about 3% of people diagnosed with chronic conditions were actually born with them.
That means that about 97% of our kids who have ADHD or a similar condition were not born with it. Instead, something in their lifestyles or environments is creating it.
Underlying stressors can lead to ADHD-like symptoms, even in individuals who do not have the condition. Additionally, for those who do have ADHD, underlying stressors can make the symptoms worse.
Therefore, recognizing and addressing underlying stressors is crucial in managing ADHD effectively.
Listed below are 5 of the most common underlying stressors that can exacerbate ADHD symptoms.
Poor Diet
Poor diet can serve as an underlying stressor for individuals with ADHD, exacerbating their symptoms significantly. Foods that are highly inflammatory, such as gluten, dairy, and soy, can lead to inflammation in the body, which can in turn exacerbate or even cause ADHD-like symptoms. Gluten is harmful for everyone (even those without ADHD or a known gluten intolerance) because it triggers increased intestinal permeability in EVERYONE, even those who don’t show an allergic response to it.
Intestinal permeability refers to the breakdown of the intestinal walls. When functioning properly, the walls of the intestines form a barrier, allowing water and nutrients to pass through but blocking other things from entering the bloodstream. When a person has increased intestinal permeability, that can lead to something called leaky gut. Leaky gut allows toxins and other harmful substances to enter the bloodstream that aren’t supposed to be there, leading to an inflammatory response in the body. This inflammation can make ADHD symptoms significantly worse. Inflammation isn’t the only issue with gluten, though. Gluten also has the potential to create opiate-like effects in some individuals. In individuals who have gut inflammation, which is very common in kids with ADHD, the enzymes in their guts are not fully breaking down gluten. What happens as a result are compounds called gluteomorphins. The protein structure of gluteomorphins is similar to that of morphine. Gluteomorphins are absorbed into the bloodstream, cross the blood brain barrier, and then bind to opiate receptors in the brain and gastrointestinal tract.
Dairy products, like gluten, are highly inflammatory and create opioid-like responses in the brain. The opioid-like protein in dairy is called casomorphin. There are two primary reasons children with ADHD should cut soy from their diets. First of all, approximately 95% of soy products come from genetically modified crops (GMOs). GMOs are linked to many health problems. They damage the digestive system and kill off the good bacteria in your gut. Because most of the soy in foods today comes from GMO plants, it’s best to cut soy out of the diet altogether. The over-production of soy is also a problem. Soy is among the largest United States farm commodities. It’s heavily processed, has a high yield, and often contains glyphosate (pesticide) residue. Because of its mass production, it is also snuck into a variety of foods at an alarming rate. The second reason to remove soy is because soy is an endocrine disruptor. When eaten in excess, it can have adverse effects on the balance of hormones in your body. It also contains isoflavones, which act like estrogen in the body. Since many breast cancers need estrogen to grow, eating an excess of soy could increase the risk of breast cancer.
Along with gluten, dairy, and soy, excess sugar can also exacerbate ADHD symptoms. Many parents overlook the importance of blood sugar management because they think of it in connection with diabetes, not ADHD. But blood sugar management is important for all of us, whether we have diabetes or not. Unstable blood sugar contributes to a whole host of problems. Read the following list of symptoms for hypoglycemia (low blood sugar), and think about how similar they are to ADHD symptoms:
- Difficulty listening
- Inability to focus or stay on task
- Being easily distracted
- Quick to get frustrated, and sometimes hard to calm down
- Unexpected anger and/or lashing out
- Unable to sit still
There are studies that suggest that the more sugar hyperactive children consume, the more destructive and restless they become. The American Heart Association recommends kids aged 2 – 18 should have less than 25 grams or six teaspoons of ADDED sugar daily. However, in my experience working with children with ADHD, this amount should be cut in half. Parents should aim to have less than 12 grams of sugar or three teaspoons of ADDED sugar daily. This does not include natural sugars found in fruits and vegetables. Along with gluten, dairy, soy, and excessive sugar, artificial flavors and colors can also exacerbate ADHD symptoms.
ADDitude magazine said this about food additives: “Food additives adversely affect a population of children with ADHD.”⁶ They went on to share 2 studies from the United Kingdom that proved food additives cause harm to children with ADHD. “In 2004, one studied healthy preschoolers after giving them either a placebo or 20 milligrams of artificial dye mix plus sodium benzoate. They found that, when the children received the actual dye and sodium benzoate, they had a significant increase in hyperactivity.” Similarly, “in 2007, a research team lead by UK researcher Donna McCann studied a group of 3-year-olds and 8- or 9-year-olds. It found that both hyperactive children and non-hyperactive children experienced increased hyperactivity scores when given artificial food colors and additives, suggesting that the dyes are a general public health concern.’” Everyone is negatively affected by artificial colors, or, as this article states, they are “a general public health concern.” A diet that is high in inflammatory foods, like gluten, dairy, soy, excessive amounts of sugar, and artificial flavors and colors, can exacerbate or sometimes even cause ADHD symptoms.
Addressing the role of diet as an underlying stressor involves adopting a nutrient-rich, balanced diet that includes whole foods, minimizing processed and sugary foods, and incorporating foods that support brain health. Replace these inflammatory foods with nutrient-dense, whole fruits and vegetables, healthy fats, and grass-fed, wild-caught protein sources. Making dietary changes and providing proper nutrition can help optimize brain function, reduce ADHD symptoms, and support overall well-being.
Vitamin & Mineral Deficiencies
Nutrient deficiencies can act as underlying stressors for individuals with ADHD, contributing to the manifestation of their symptoms. Certain nutrients play a crucial role in brain function, neurotransmitter production, and overall cognitive health. For example, deficiencies in omega-3 fatty acids, zinc, magnesium, iron, and B vitamins have been associated with an increased risk of ADHD symptoms. Omega-3 fatty acids, found in fatty fish, flaxseeds, and walnuts, are essential for brain development and function. Zinc and magnesium are involved in neurotransmitter regulation and can affect attention and impulse control. Iron is necessary for optimal cognitive function, and B vitamins, including B6 and B12, play a role in neurotransmitter synthesis. When these nutrients are deficient, it can disrupt neural pathways and neurotransmitter balance, potentially exacerbating ADHD symptoms.
Addressing nutrient deficiencies through a balanced and nutrient-dense diet or targeted supplementation under the guidance of a healthcare professional can help alleviate underlying stressors and support better management of ADHD symptoms. In 2017, a study⁷ concluded that the addition of micronutrients in the diet improved overall function, reduced impairments, and improved attention, emotional regulation and aggression.
Gut Break Down
The digestive system (aka the gut) is responsible for receiving food, breaking it down, extracting the nutrients, and discarding the junk. If at any point in doing these things, the digestive system is impaired, it wreaks havoc on the entire body. Research suggests that there is a strong connection between gut health and ADHD symptoms. The gut is home to trillions of bacteria, collectively known as the gut microbiota, which play a crucial role in various aspects of our health, including brain function and mental well-being.
When there is an imbalance in the gut microbiota, often referred to as dysbiosis, it can lead to gut breakdown and the release of harmful byproducts into the bloodstream. This process can trigger inflammation and oxidative stress, both of which have been associated with ADHD symptoms.
Furthermore, the gut microbiota produce and regulate neurotransmitters, such as serotonin and dopamine, which are essential for mood regulation, attention, and impulse control. When the gut microbiota are imbalanced, it can disrupt neurotransmitter production and signaling, potentially exacerbating ADHD symptoms. Therefore, addressing gut health through dietary modifications, probiotics, and lifestyle changes may help reduce gut breakdown, alleviate inflammation, and support better management of ADHD symptoms. Leaky gut⁸, as already mentioned under Poor Diet, can be caused by parasites, toxic exposure, medication, gluten, food intolerances, or other underlying stressors.
Leaky gut⁹ is when food particles slip through the intestinal walls and head into the bloodstream. When this occurs, the body recognizes these food particles as foreign matter and then creates an immunological response.¹⁰ If the gut isn’t functioning properly, many other areas of the body are affected, not the least of which is ADHD.
Kryptopyrrole
Pyrroles are a normal chemical byproduct in the body. They attach to vitamin B6 and zinc and draw these elements out of the body when they’re excreted through the urine. If someone has elevated urine kryptopyrrole levels, it can result in a dramatic deficiency of zinc and vitamin B6.
A high Kryptopyrrole result is also known as pyroluria, pyrrole disorder, or elevated pyrroles and is a condition that affects the metabolism of certain nutrients, particularly zinc and vitamin B6. While the direct link between kryptopyrrole and ADHD is still being explored, some studies and anecdotal evidence suggest that individuals with ADHD (as well as those with behavior disorders, depression, and aggressive behavior) may have higher levels of kryptopyrrole. Elevated levels of kryptopyrrole can lead to deficiencies in essential nutrients like zinc and vitamin B6, which are crucial for neurotransmitter function and brain health. These nutrient deficiencies can potentially exacerbate ADHD symptoms, as they play a role in supporting cognitive function, mood regulation, and attention span. Additionally, zinc and vitamin B6 are involved in the synthesis and regulation of neurotransmitters like dopamine and serotonin, which are important for maintaining focus and managing impulses.
Some of the symptoms common to pyroluria include the following:
-
Poor tolerance to physical / emotional stress
-
Irritability
-
Anxiety
-
Poor anger control
-
Emotional mood swings
-
Sensitivity to light or sound
-
Poor short-term memory
Addressing kryptopyrrole levels through targeted nutrient supplementation and a balanced diet may help restore nutrient balance and potentially alleviate ADHD symptoms in individuals with this condition, in particular in regard to emotional regulation. However, it is important to consult with a healthcare professional for proper diagnosis and personalized treatment approaches.
Toxin Exposure
Toxin exposure can have a significant impact on individuals with ADHD, potentially exacerbating their symptoms. The human body is constantly exposed to various toxins from the environment, including pollutants, heavy metals, pesticides, and certain chemicals. These toxins can disrupt the normal functioning of the nervous system and interfere with the development and regulation of neurotransmitters in the brain, which are crucial for attention, focus, and impulse control.
Research suggests that children with higher levels of toxin exposure, such as lead or mercury, may be more likely to exhibit ADHD-like symptoms. Additionally, certain toxins can contribute to inflammation and oxidative stress in the body, further affecting cognitive function and behavior. Minimizing exposure to toxins, such as by avoiding environmental pollutants, choosing organic foods, and using natural cleaning and personal care products, may help reduce the impact on individuals with ADHD.
Furthermore, supporting the body’s natural detoxification processes through a healthy diet, regular exercise, and proper hydration can aid in the removal of toxins and potentially alleviate ADHD symptoms.
ADHD at School
Does ADHD Affect School?
ADHD can significantly impact a child’s experience in school. The core symptoms of inattention, hyperactivity, and impulsivity can make it challenging for children with ADHD to concentrate, follow instructions, complete tasks, and stay organized. They may struggle to maintain focus during lectures or while working on assignments, leading to difficulty retaining information and lower academic performance.
Additionally, their impulsivity may result in impulsive behaviors or speaking out of turn, disrupting the classroom environment. These difficulties can lead to academic underachievement, poor self-esteem, and increased frustration for children with ADHD.
However, with appropriate support, accommodations, and strategies tailored to their individual needs, children with ADHD can thrive academically and succeed in school. It is essential for teachers, parents, and school personnel to work collaboratively to create an inclusive and supportive learning environment that addresses the specific challenges associated with ADHD.
Two valuable tools that can help students be successful in the school environment are 504 Plans and/or Individualized Education Programs.
504 Accommodation Plan
A 504 plan is a valuable tool for students with ADHD to receive the necessary support and accommodations in an educational setting. Designed under Section 504 of the Rehabilitation Act of 1973, this plan ensures that students with disabilities, including ADHD, have equal access to education. A 504 plan outlines specific accommodations and modifications to help students with ADHD manage their symptoms and succeed academically. These may include preferential seating, extended time for assignments or tests, frequent breaks, access to assistive technology, and additional support from teachers or staff. The plan is typically developed by a team that includes parents, teachers, school administrators, and relevant professionals. It provides a framework for collaboration and communication among all involved parties, ensuring that the student’s needs are understood and met. By implementing a 504 plan, schools can provide the necessary support and create an inclusive environment where students with ADHD can thrive and reach their full potential.
Individual Education Plan (IEP)
An Individualized Education Program (IEP) is another tool for students with ADHD to receive comprehensive and tailored support in their educational journey.
Developed under the Individuals with Disabilities Education Act (IDEA), an IEP is a legal document that outlines the specific goals, accommodations, modifications, and services required to meet the unique needs of a student with ADHD.
The IEP team, which includes parents, teachers, special education professionals, and other relevant individuals, collaboratively creates the plan. The IEP addresses various aspects of the student’s education, such as academic goals, behavior management strategies, classroom accommodations, specialized instruction, and related services. It ensures that the student receives appropriate educational interventions and support to navigate challenges associated with ADHD.
By implementing an IEP, schools provide a structured and supportive environment that maximizes the student’s learning potential and promotes their overall academic and personal growth. The IEP serves as a roadmap for educators to individualize instruction and support, empowering students with ADHD to thrive in the educational setting and achieve their educational goals.
ADHD Treatment
ADHD Medication For Kids
There are several types of medications commonly prescribed for the treatment of ADHD (Attention-Deficit/Hyperactivity Disorder). For some children, these medications can help manage the symptoms of ADHD and improve focus, attention, and impulse control.
Stimulant Medications:
Stimulants are the most commonly prescribed medications for ADHD. They work by increasing the levels of certain chemicals in the brain, such as dopamine and norepinephrine, which help regulate attention and behavior. Commonly prescribed stimulant medications include methylphenidate (Ritalin, Concerta) and amphetamine-based medications (Adderall, Vyvanse).
Non-Stimulant Medications:
Non-stimulant medications are an alternative for individuals who may not tolerate or respond well to stimulants. These medications work differently than stimulants and typically target norepinephrine levels in the brain. Non-stimulant medications commonly used for ADHD include atomoxetine (Strattera), guanfacine (Intuniv), and clonidine (Kapvay).
For many families, medication is the only option offered upon an ADHD diagnosis, and this is unfortunate. Parents are not often told about natural strategies that can be effective at reducing ADHD symptoms.
Though medication can be effective for some children, medication can also show little effect (or even create more issues) for other children.
One thing to keep in mind is that medication is not a quick fix. Parents sometimes assume it will be, but it rarely happens. It can take months – sometimes even years – to find the right medication and dosage.
Caregivers have to navigate side effects and track behaviors to see which medication is working and which one isn’t. They have to schedule doctors’ appointments on a regular basis to discuss their findings and evaluate symptoms. As children grow, dosages change. Sometimes, medications that once worked effectively stop working. It’s important to realize that no matter what treatment plan a parent might choose, there is no quick fix.
It’s also important to remember that each child is unique. Therefore, ADHD management should be tailored for each individual.
ADHD Medication Side Effects
ADHD (Attention-Deficit/Hyperactivity Disorder) medications, like any other medication, can have potential side effects. The specific side effects may vary depending on the type of medication prescribed. Common side effects associated with ADHD medications include:
Stimulant Medications:
• Decreased appetite
• Difficulty falling asleep or staying asleep
• Stomachache
• Headache
• Increased heart rate
• Increased blood pressure
• Mood swings
• Irritability
• Emotional changes
Non-Stimulant Medications:
• Drowsiness
• Stomach upset
• Dizziness
• Dry mouth
• Constipation
• Changes in blood pressure or heart rate
Medication is not the only option to treat ADHD symptoms. There are also natural strategies that can be effective.
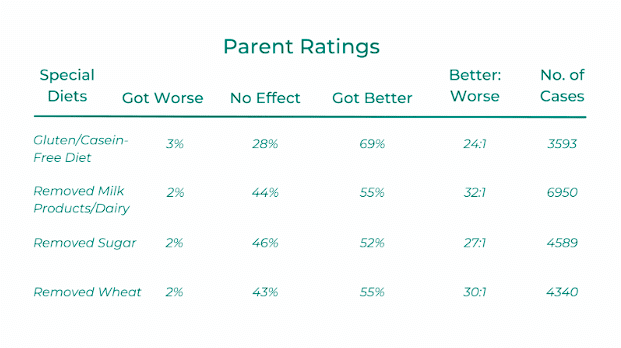
How to Help a Child with ADHD Without Medication
As mentioned above, there are natural strategies that can be as effective (at times, even more effective) than medication at supporting a child with ADHD. In a study conducted by the Autism Research Institute¹¹, the researchers compared the behavioral effects of different types of interventions to see which ones were most effective. To do this, they looked at data they had been collecting from parents since 1967. They reviewed interventions such as Amphetamine medication, antibiotics, antifungals, sleeping medicines, SSRIs, certain vitamins and supplements, and various special diets. The researchers collated the responses and combined them into three categories: symptoms were made worse, treatment had no effect, or symptoms were made better. The “Better to Worse” column gives the number of children who “Got Better” compared to each child who “Got Worse.” With many of the common ADHD medications, for every child who got better, another got worse. In contrast, parents who implemented a Gluten-Free and Casein-Free diet for their children showed a 24:1 ratio. That means that for every 24 kids who got better, only 1 child got worse. Similarly, parents who removed sugar saw a 27:1 ratio, meaning that 27 children improved, while only one child worsened.
ADHD Diet
A study in 2011¹² concluded that 64 percent of children diagnosed with ADHD were actually experiencing a hypersensitivity to food. Another study showed that 56% of ADHD kids tested positive for food allergies compared to less than 8% of kids in the general population.¹³ There is a clear correlation between ADHD and food allergies. Nonetheless, most doctors don’t even mention this correlation to caregivers.
In 2002, a study¹⁴ was done to show the connection between food intolerances and depression. The study concluded that the patient’s symptoms of depression considerably improved while on an elimination diet. Granted, this study was about depression, not ADHD, but considering what we know about the neurotransmitters that are made in the gut (serotonin and dopamine), it makes sense that if a similar study were conducted on patients with ADHD, there would likely be similar results.
In 2015, a study¹⁵ showed the risk of hyperactivity increased by 14% with each additional sweetened beverage. It also correlated soda consumption with higher aggression. And yet, even though these are two common symptoms of ADHD in children, caregivers are rarely told to avoid soda.
In 2017, a study¹⁶ concluded that the addition of micronutrients in the diet improved overall function, reduced impairments, and improved attention, emotional regulation and aggression.
Clearly, medication is NOT the only way to help children with ADHD. All of these studies strongly suggest that diet matters and that diet can be an effective natural way to reduce ADHD symptoms.
As mentioned in the Poor Diet section above, there are several foods that – when removed from the diet – can reduce inflammation in the body, brain, and gut. These foods include gluten, dairy, soy, artificial flavors and colors, and excessive amounts of sugar.
BUT, the ADHD diet is not only about foods to remove, but also about foods to incorporate.
Some micronutrient-rich whole foods that should be incorporated into the diet include the following:
- Vegetables (like carrots, broccoli, cauliflower, spinach, kale, peppers, brussel sprouts, asparagus, green beans, etc).
- Fruits (like blueberries, raspberries, bananas, apples, grapes, blackberries, cherries, oranges, mangos, pears, etc).
- Beans
- Eggs
- Wild-Caught Fish
- Nuts and seeds
- Gluten-free grains (like quinoa, rice, and gluten-free oats)
- Healthy fats (like avocado, olive, and coconut oil)
- Grass-fed organic animal protein (like beef, chicken, turkey, and collagen)
In addition to these foods, water is vital in the healing journey. Water carries nutrients to cells, helps the body flush out waste, enables the body to dissolve minerals so they are accessible throughout, and does a variety of other important functions.¹⁷ It also aids in detoxification, which is critical for our children with compromised systems.
According to the American Academy of Pediatrics, “children ages 1-3 years need approximately 4 cups of beverages per day…This increases for older kids to around 5 cups for 4-8 year olds, and 7-8 cups for older children.”¹⁸
ADHD Supplements
Supplements can play a supportive role in managing ADHD symptoms, although they are not a replacement for comprehensive treatment. They can never be the be-all-and-end-all for ADHD symptom reduction. It’s important to remember that you can’t supplement your way out of a poor diet. Nonetheless, certain supplements have shown promise in addressing specific aspects of ADHD, such as improving focus, attention, and mood.
ADHD Supplement – Omega 3
A good quality fish oil for Omega 3 fatty acids can be beneficial for children with ADHD. Omega-3 and Omega-6 fatty acids are polyunsaturated fatty acids that our bodies cannot make on their own. That means the only way we obtain these types of fat is through diet or supplementation.
Omega-3 fatty acids can be found in oily fish like salmon, trout, mackerel, tuna, and sardines, nuts like almonds, walnuts, hazelnuts, and pecans, and seeds like chia, flax, and pumpkin seeds. Omega-6 fatty acids are found in many plant-based oils.
Omega-3 and Omega-6 fatty acids are meant to be in a one-to-one ratio in the body. Unfortunately, due to the Western diet, the amount of Omega 6 in our bodies has reached unprecedented proportions and results in inflammation, blood pressure issues, and heart disorders. In contrast, Omega-3, which comes from a Mediterranean diet, is typically extremely low in Americans.¹⁹
This deficiency of Omega-3 fatty acids is correlated to ADHD in children. Paul Montgomery, D. Phil., a researcher at the University of Oxford in England, gave school-age children fish oil supplementation for three months to help boost their Omega-3 intake. At the end of that time, he found that those taking the supplements showed improvement in behavior, as well as in reading and spelling. He concluded in Pediatrics that “a lack of certain polyunsaturated fatty acids may contribute to dyslexia and attention-deficit/hyperactivity disorder.”²⁰
Research²¹ suggests this deficiency in Omega-3 fatty acids can be improved by incorporating foods that naturally contain fatty acids such as fish and nuts. Unfortunately, many children refuse to eat these types of food, preferring to stick with other, more kid-friendly dishes. Because of this, supplementation is often helpful.
ADHD Supplement – Vitamin D
Vitamin D is another supplement that can be beneficial for children with ADHD. It is especially effective when taken with a supplement of Omega-3 fatty acids. That’s because these nutrients play a vital role in our serotonin production. Serotonin is our feel-good hormone and is closely tied to behavior, appetite, sleep, digestion, and memory, all things that many children with ADHD battle. Vitamin D also helps reduce inflammation in the body. As mentioned, inflammation in the body affects much more than just gut health. Once that inflammation reaches the brain, it can also create behavior issues, hyperactivity, anger issues, problems with memory, etc. One of the best natural ways to get more vitamin D is to get outside in the sunlight, but since this is not always possible, a vitamin D supplement can be very beneficial. Other food sources for vitamin D include oily fish, cod liver oil, mushrooms, and egg yolks.
ADHD Supplement – Probiotics
The brain has many areas that are involved in gut function, but one of the main areas is the frontal lobe. The frontal lobe talks to the gut via nerve branches and two way chemical messengers. It is involved in things like attention, focus, executive function, planning, organizing, and problem solving, all of which are common symptoms of many of our children with ADHD. When we ensure that our children’s guts are functioning well, we simultaneously ensure their frontal lobes are functioning well too. That’s why probiotics can be so beneficial for children with ADHD. Probiotics can be found naturally in Kombucha, dark chocolate, and fermented foods, or come in supplement form. Research²² shows that taking probiotics that contain a certain type of gut bacteria can reduce inflammation in the body,²³ help detoxify, reduce anxiety, improve mood, and also protect the body against the damaging mental and physical effects of stress.²⁴
ADHD Supplement – Magnesium
Magnesium is used in over three hundred biochemical processes in the body, and it is an important element that supports muscles, helps with relaxation, aids restful sleep, keeps hormonal balance, keeps the heartbeat steady, regulates blood glucose levels, and aids in the production of energy. Stress depletes magnesium levels, so if a child is already low in magnesium and experiences stress, that anxiety can make their magnesium levels even lower. It’s a vicious cycle, but one that can be supported through eating magnesium-rich foods like spinach, asparagus, cabbage, avocado, bananas, seeds, nuts, peas, broccoli, dark chocolate, or oily fish. It can also be supported through supplementation.
Many caregivers find that magnesium makes a surprising difference to their kids’ anxiety or depression, aids in sleep, and also reduces hyperactivity. Research suggests that children with ADHD often have low magnesium levels, and using supplements can have a calming effect on behavior²⁵ and reduce insomnia, agitation, and muscle cramps. With magnesium, it’s important to remember that it can take a couple of weeks to up to a month to build up in the body, so don’t expect immediate results.
ADHD Supplement -Iron
Many people only associate low levels of iron with anemia, but iron is critical for optimal brain function. Some researchers also believe that low levels of iron can be an underlying stressor for ADHD. In one particular study, iron-deficient ADHD children were given iron supplements. These children saw improvement in their ADHD symptoms, as compared to the children who did not receive the supplementation.²⁶ Some foods that are naturally high in iron include the following: lean beef and poultry, oysters and shellfish, cashews, pumpkin seeds, quinoa, spinach, broccoli, and dark chocolate. If you believe your child might have low levels of iron, consider whether or not supplementation might be beneficial.
ADHD Supplements – Others
Additional supplements that can be beneficial for supporting children with ADHD include the following:
- Zinc
- Calcium
- B6
- Folate & B12
- Vitamin C
- Selenium
- Digestive Enzymes
Exercise for ADHD
Exercise offers numerous benefits for individuals with ADHD, making it a valuable addition to their management plan. Engaging in regular physical activity has been shown to improve attention, mental focus, behavior, memory, academic performance, and cognitive function, which are often areas of challenge for people with ADHD. Physical activity may improve executive function by altering brain structure and function, particularly in the frontal region of the brain, which is responsible for attention, focus, memory, movement, and learning.
Exercise increases the production of neurotransmitters like dopamine, norepinephrine, and serotonin, which play a crucial role in regulating attention and mood. These neurotransmitters are often dysregulated in individuals with ADHD, and exercise can help rebalance their levels. Moreover, exercise provides an outlet for excess energy, helping to reduce hyperactivity and impulsivity. It promotes better sleep patterns, which can have a positive impact on attention and behavior during the day. Additionally, participating in sports or physical activities can enhance self-esteem, social skills, and peer interactions.
Overall, regular exercise can improve ADHD symptoms, boost overall well-being, and contribute to a more balanced and fulfilling life. It is important to provide children and adolescents opportunities and encouragement to participate in physical activities that are appropriate for their age, that are enjoyable, and that offer variety. According to the U.S. Department of Health & Human Services physical activity guidelines, preschool-aged children (ages 3 through 5 years) should be physically active throughout the day to enhance growth and development and children and adolescents (ages 6 through 17 years) should do 60 minutes or more of moderate-to-vigorous physical activity daily.
ADHD Parent Training
“Typical” parenting strategies don’t always work with children with ADHD As a result, ADHD-specific parent training can be beneficial for parents of children with ADHD. ADHD-specific parenting practices focus on understanding and addressing the unique needs and challenges of children with ADHD.
- It empowers parents to look below the surface of their child’s behaviors, discovering the sources of the child’s difficulties.
- It holds knowledge on how nutrition, parenting, family stressors, the environment, and certain school settings can actually exacerbate ADHD symptoms.
- It deepens your understanding of how your child’s nervous system contributes to their behaviors, emotions, and difficulties.
- It focuses on expanding your awareness of your child’s emotional, physical and relational needs and how to respond to these vs. focusing on ‘managing’ their behaviors.
- It supports your children to develop their self-regulation through your relational connection and co-soothing.
- It is about growing & learning new ways of being and connecting with your child.
Comorbidities
ADHD, or Attention-Deficit/Hyperactivity Disorder, is often accompanied by comorbidities, which are additional mental health conditions that coexist with ADHD.
Some common comorbidities of ADHD include anxiety disorders, such as generalized anxiety disorder and social anxiety disorder, which can intensify feelings of worry and unease. Depression is also frequently seen in individuals with ADHD, contributing to persistent feelings of sadness and low mood. Learning disabilities and specific learning disorders may co-occur with ADHD, affecting academic performance and the acquisition of certain skills. Other comorbidities may include oppositional defiant disorder (ODD), conduct disorder, autism spectrum disorder (ASD), and tics or Tourette’s syndrome.
It is important to recognize and address these comorbidities, as they can impact various aspects of an individual’s life and require tailored treatment approaches that target both ADHD symptoms and the accompanying conditions.
ADHD & Autism
ADHD and autism spectrum disorder (ASD) are two distinct neurodevelopmental conditions that can coexist and be comorbid in some individuals. While they are separate diagnoses, research has shown that there is a higher prevalence of ADHD symptoms among individuals with ASD compared to the general population. The co-occurrence of ADHD and autism can present unique challenges for individuals, as they may experience difficulties with attention, impulsivity, hyperactivity, social interactions, and communication skills. The presence of both conditions can impact various aspects of daily functioning, including academic performance, social relationships, and overall well-being. It is important to recognize and understand the comorbidity of ADHD and autism to provide comprehensive and individualized support and interventions for individuals who may be affected by both conditions. Proper assessment and diagnosis by qualified professionals are essential in order to develop tailored treatment plans that address the specific needs and challenges associated with ADHD and autism comorbidity, promoting optimal development and improved quality of life for individuals affected by these conditions.
ADHD & Anxiety
ADHD and anxiety are frequently observed as comorbid conditions, meaning they often coexist in individuals. Many individuals diagnosed with ADHD also experience symptoms of anxiety, such as excessive worry, restlessness, racing thoughts, and feelings of tension or unease. Similarly, individuals with anxiety disorders may exhibit difficulties with attention, impulsivity, and hyperactivity, which are characteristic of ADHD. The presence of both ADHD and anxiety can significantly impact various areas of a person’s life, including academic performance, social interactions, and overall emotional well-being. Understanding the comorbidity of ADHD and anxiety is crucial for accurate diagnosis and effective treatment. It is important to address both conditions simultaneously and provide appropriate interventions that address the unique needs and challenges associated with each. A comprehensive approach that combines behavioral interventions, therapy, and, in some cases, medication management can help individuals manage symptoms of both ADHD and anxiety, improving their overall functioning and quality of life.
Tics & ADHD
ADHD and tics are commonly observed as comorbidities, meaning they often coexist in individuals. Tics refer to sudden, repetitive, and involuntary movements or vocalizations. Studies have shown that individuals with ADHD are more likely to experience tics compared to the general population. The presence of both ADHD and tics can present unique challenges for individuals, as tics can be disruptive and affect daily functioning. It is important to recognize and address both conditions when evaluating and managing symptoms. Treatment approaches may involve a combination of strategies, including behavioral interventions, therapy, and, in some cases, medication management. Understanding the comorbidity of ADHD and tics is crucial for providing comprehensive care and tailored interventions that address the specific needs of each individual, promoting improved functioning and quality of life.
ODD & ADHD
ADHD and Oppositional Defiant Disorder (ODD) are frequently observed as comorbidities, often occurring together in individuals. ODD is characterized by a persistent pattern of defiant, disobedient, and hostile behavior toward authority figures. It is estimated that a significant number of children with ADHD also meet the criteria for ODD. The presence of both conditions can make it more challenging for individuals to manage their behavior and emotions, leading to difficulties in various settings, including home and school. Treatment for comorbid ADHD and ODD may involve a comprehensive approach that combines behavioral interventions, parent training, counseling, and, in some cases, medication. By addressing both ADHD and ODD, professionals can provide more targeted and effective interventions that support improved behavior regulation, social interactions, and overall functioning for individuals experiencing these comorbid conditions.
Conclusion
Understanding ADHD in its entirety – from its types and symptoms to its underlying stressors and treatment options – is crucial for effective management and support. ADHD manifests differently in each person, making personalized approaches essential. It’s also important to remember that there are various natural strategies, like dietary changes and exercise, that can significantly improve ADHD symptoms. If you’re looking for more resources or support in your ADHD journey, remember that ADHD Thrive Institute is here to provide comprehensive guidance tailored to your unique needs and challenges. Join us in exploring effective ways to reduce ADHD symptoms naturally and enhance the quality of life for those affected by this condition.
Resources List
¹ ADDitude editors, “ADHD Statistics: New ADD Facts and Research.” ADDitude, https://www.additudemag.com/statistics-of-adhd/. Medically Reviewed by Sharon Saline, Psy.D., Updated on May 24, 2023. Accessed 20 June 2023.
² Melissa L. Danielson, Rebecca H. Bitsko, Reem M. Ghandour, Joseph R. Holbrook, Michael D. Kogan & Stephen J. Blumberg. (Jan. 24, 2018). Prevalence of Parent-Reported ADHD Diagnosis and Associated Treatment Among U.S. Children and Adolescents, 2016. Journal of Clinical Child & Adolescent Psychology, 47:2, 199-212, DOI: 10.1080/15374416.2017.1417860. Retrieved from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5834391/pdf/nihms937906.pdf
³ American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC. https://doi.org/10.1176/appi.books.9780890425596.
⁴ Polanczyk G., De Lima M.S., Horta B.L., Biederman J., Rohde L.A. (2007). The Worldwide Prevalence of ADHD: A Systematic Review and Metaregression Analysis. AM J Psychiatry 164:942–948. Retrieved from: https://ajp.psychiatryonline.org/doi/full/10.1176/ajp.2007.164.6.942?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed
⁵ “Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR).” Psychiatry.org, https://www.psychiatry.org/dsm5. Accessed 20 June 2023.
⁶ https://www.additudemag.com/feed-your-childs-focus-adhd-food-nutrition/ Laura Stephens, M.Sci. accessed June 21, 2023, updated March 31, 2022.
⁷Rucklidge JJ;Eggleston MJF;Johnstone JM;Darling K;Frampton CM; “Vitamin-Mineral Treatment Improves Aggression and Emotional Regulation in Children with ADHD: A Fully Blinded, Randomized, Placebo-Controlled Trial.” Journal of Child Psychology and Psychiatry, and Allied Disciplines, U.S. National Library of Medicine, 2 Oct. 2017, https://pubmed.ncbi.nlm.nih.gov/28967099/. Accessed 07 Jan 2022.
⁸ Bell, Becky. “Is Leaky Gut Syndrome a Real Condition? an Unbiased Look.” Healthline, Healthline Media, 2 Feb. 2017, https://www.healthline.com/nutrition/is-leaky-gut-real#TOC_TITLE_HDR_2. Accessed 07 Jan 2022.
⁹ Unfortunately, even though there is significant evidence supporting the understanding of leaky gut, mainstream medical professionals sometimes deny its existence. Because of this, leaky gut alone is not a diagnosable condition. Medical professionals do, however, agree that increased intestinal permeability is a problem that can lead to chronic conditions.
¹⁰ Buckley, Aaron, and Jerrold R Turner. “Cell Biology of Tight Junction Barrier Regulation and Mucosal Disease.” Cold Spring Harbor Perspectives in Biology, Cold Spring Harbor Laboratory Press, 2 Jan. 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5749156/. Accessed 02 Feb 2022.
¹¹ Parent Ratings of Behavioral Effects of Biomedical Interventions. Autism Research Institute, Mar. 2009, https://www.autism.org/treatment-ratings-for-autism/ and https://www.autism.org/wp-content/uploads/2018/12/ParentRatings2009.pdf. Accessed 07 Jan 2022.
¹² Pelsser, Dr. Lidy M, et al. “Effects of a Restricted Elimination Diet on the Behaviour of Children with Attention-Deficit Hyperactivity Disorder (INCA Study): a Randomised Controlled Trial.” The Lancet, 5 Feb. 2011, https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(10)62227-1/fulltext. Accessed 06 Jan 2022.
¹³ “ADHD (Attention Deficit and Hyperactivity Disorder).” Food for the Brain, 9 Nov. 2020, https://foodforthebrain.org/condition/adhd-and-hyperactivity/. Accessed 06 Jan 2022.
¹⁴ Parker, Gordon, and Tim Watkins. “Treatment-Resistant Depression: When Antidepressant Drug Intolerance May Indicate Food Intolerance.” The Australian and New Zealand Journal of Psychiatry, U.S. National Library of Medicine, Apr. 2002, https://pubmed.ncbi.nlm.nih.gov/11982551/. Accessed 06 Jan 2022.
¹⁵ Schwartz DL; Gilstad-Hayden K;Carroll-Scott A;Grilo SA;McCaslin C;Schwartz M;Ickovics JR; “Energy Drinks and Youth Self-Reported Hyperactivity/Inattention Symptoms.” Academic Pediatrics, U.S. National Library of Medicine, 9 Feb. 2015, https://pubmed.ncbi.nlm.nih.gov/25676784/. Accessed 07 Jan 2022.
¹⁶ Rucklidge JJ;Eggleston MJF;Johnstone JM;Darling K;Frampton CM; “Vitamin-Mineral Treatment Improves Aggression and Emotional Regulation in Children with ADHD: A Fully Blinded, Randomized, Placebo-Controlled Trial.” Journal of Child Psychology and Psychiatry, and Allied Disciplines, U.S. National Library of Medicine, 2 Oct. 2017, https://pubmed.ncbi.nlm.nih.gov/28967099/. Accessed 07 Jan 2022.
¹⁷ “Water: Essential to Your Body.” Mayo Clinic Health System, 22 July 2020, https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/water-essential-to-your-body. Accessed 28 Oct 2021.
¹⁸ Rethy, Janine. “Choose Water for Healthy Hydration.” HealthyChildren.org, 27 Jan. 2020, https://www.healthychildren.org/English/healthy-living/nutrition/Pages/Choose-Water-for-Healthy-Hydration.aspx. Accessed 28 Oct 2021.
¹⁹ Walle, Gavin Van De. “Polyunsaturated Fat: Definition, Foods, Benefits and Risks.” Healthline, Healthline Media, 31 Oct. 2018, https://www.healthline.com/nutrition/polyunsaturated-fat#risks. Accessed 23 Nov 2021.
²⁰ Hallowell, Edward, et al. “Can a Daily Fish Oil Supplement Help Curb Symptoms of ADHD?” ADDitude, ADDitude, Updated Jan 5, 2022, https://www.additudemag.com/fish-oil-for-adhd-symptoms/. Accessed 23 Nov 2021.
²¹ LaChance, Laura, et al. “Omega-6 to Omega-3 Fatty Acid Ratio in Patients with ADHD: A Meta-Analysis.” Journal of the Canadian Academy of Child and Adolescent Psychiatry = Journal De L’Academie Canadienne De Psychiatrie De L’enfant Et De L’adolescent, 1719-8429, 2016, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4879948/. Accessed 23 Nov 2021.
²² Bear, Tracey L K, et al. “Role of the Gut Microbiota in Dietary Interventions for Depression and Anxiety.” OUP Academic, Oxford University Press, 9 Mar. 2020, https://academic.oup.com/advances/article/11/4/890/5801053?login=true. Accessed 04 Feb 2022.
²³ Plaza-Díaz, Julio, et al. “Evidence of the Anti-Inflammatory Effects of Probiotics and Synbiotics in Intestinal Chronic Diseases.” Nutrients, MDPI, 28 May 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5490534/. Accessed 04 Feb 2022.
²⁴ Yaghoubfar, Rezvan, et al. “Modulation of Serotonin Signaling/Metabolism by Akkermansia Muciniphila and Its Extracellular Vesicles through the Gut-Brain Axis in Mice.” Nature News, Nature Publishing Group, 17 Dec. 2020, https://www.nature.com/articles/s41598-020-79171-8. Accessed 04 Feb 2022.
²⁵ Starobrat-Hermelin, B, and T Kozielec. “The Effects of Magnesium Physiological Supplementation on Hyperactivity in Children with Attention Deficit Hyperactivity Disorder (ADHD). Positive Response to Magnesium Oral Loading Test.” Magnesium Research, U.S. National Library of Medicine, https://pubmed.ncbi.nlm.nih.gov/9368236/. Accessed 24 Nov 2021.
²⁶ Konofal E;Lecendreux M;Deron J;Marchand M;Cortese S;Zaïm M;Mouren MC;Arnulf I; “Effects of Iron Supplementation on Attention Deficit Hyperactivity Disorder in Children.” Pediatric Neurology, U.S. National Library of Medicine, Jan 2008, https://pubmed.ncbi.nlm.nih.gov/18054688/. Accessed 28 Jan 2022.