Is this normal… or is it ADHD?
It’s a question that keeps many parents up at night, especially those raising a child who’s impulsive, sensitive, intense, or constantly in motion.
Is this just a phase? Just their personality? Or is it something more?
One mom I work with said it best: “When the school finally stopped calling every day, I didn’t feel relief. I panicked. I was so used to chaos, I didn’t know how to trust the calm.”
If you’ve ever felt that way too–like your nervous system can’t relax even when things are going well—you’re far from abnormal. I see it all the time in the families I support, and I even experienced it myself with my own son who has ADHD.
You’ve made progress. But one bad day, one meltdown, one phone call from school… and suddenly you’re back in that spiral again, wondering:
“Is this behavior normal, or are we slipping backwards?”
In this post, we’re going to unpack that question and give you real, practical tools to help you tell the difference between developmentally typical behavior and ADHD. Because yes, ADHD is real. But not every big emotion, meltdown, or hard day is a symptom of it.
Whether your child is in kindergarten or entering their teen years, this guide will help you trust your instincts, track meaningful patterns, and understand what your child’s body and behavior might really be trying to say.
👉 Prefer to listen instead of read? [Listen to the podcast episode on this same topic here]
What’s Normal Behavior…And What’s Not?
Let’s get one thing straight: kids are messy.
They forget things. They interrupt. They roll their eyes, get obsessed with dinosaurs or Minecraft, make weird noises, and sometimes melt down over the “wrong” socks. That’s developmentally appropriate.
Especially in elementary and early teen years, the brain is still under construction. The prefrontal cortex (the part of the brain responsible for focus, impulse control, emotional regulation, and decision-making) isn’t fully developed until around age 22 to 25.
So yes, your 7-year-old might cry because their sandwich was cut the “wrong” way. Your 12-year-old might talk non-stop and forget their lunch three days in a row. And your 15-year-old might have a strong emotional reaction when they’re overwhelmed.
Those things can all be normal.
But here’s the difference between normal behavior and a pattern that may point to something deeper, like ADHD:
Normal is occasional forgetfulness.
✘ Concerning is never remembering basic instructions, even with support.
Normal is emotional outbursts during stress or transitions.
✘ Concerning is daily meltdowns over small changes.
Normal is fidgeting or talking in class.
✘ Concerning is chronic disruption, inability to complete tasks, or focus, despite structure and accommodations.

It’s not about perfection. It’s about patterns, frequency, intensity, and how much the behavior is interfering with your child’s ability to thrive at home, in school, and in relationships.
What to Do If You’re Not Sure
Now, maybe you’re reading this and thinking, “I still don’t know… Is this ADHD? Or is it just a phase?” I want to encourage you to think about what your gut is telling you.
Remember, you are your child’s best expert. You know your child better than anyone else – better than a teacher, a doctor, or even a well-meaning relative with lots of opinions.
So when your intuition says, “Something feels off…” trust that. You might not know exactly what it is yet, but your awareness is already pointing you in the right direction.
Instead of jumping straight to “Is this ADHD?” try this instead:
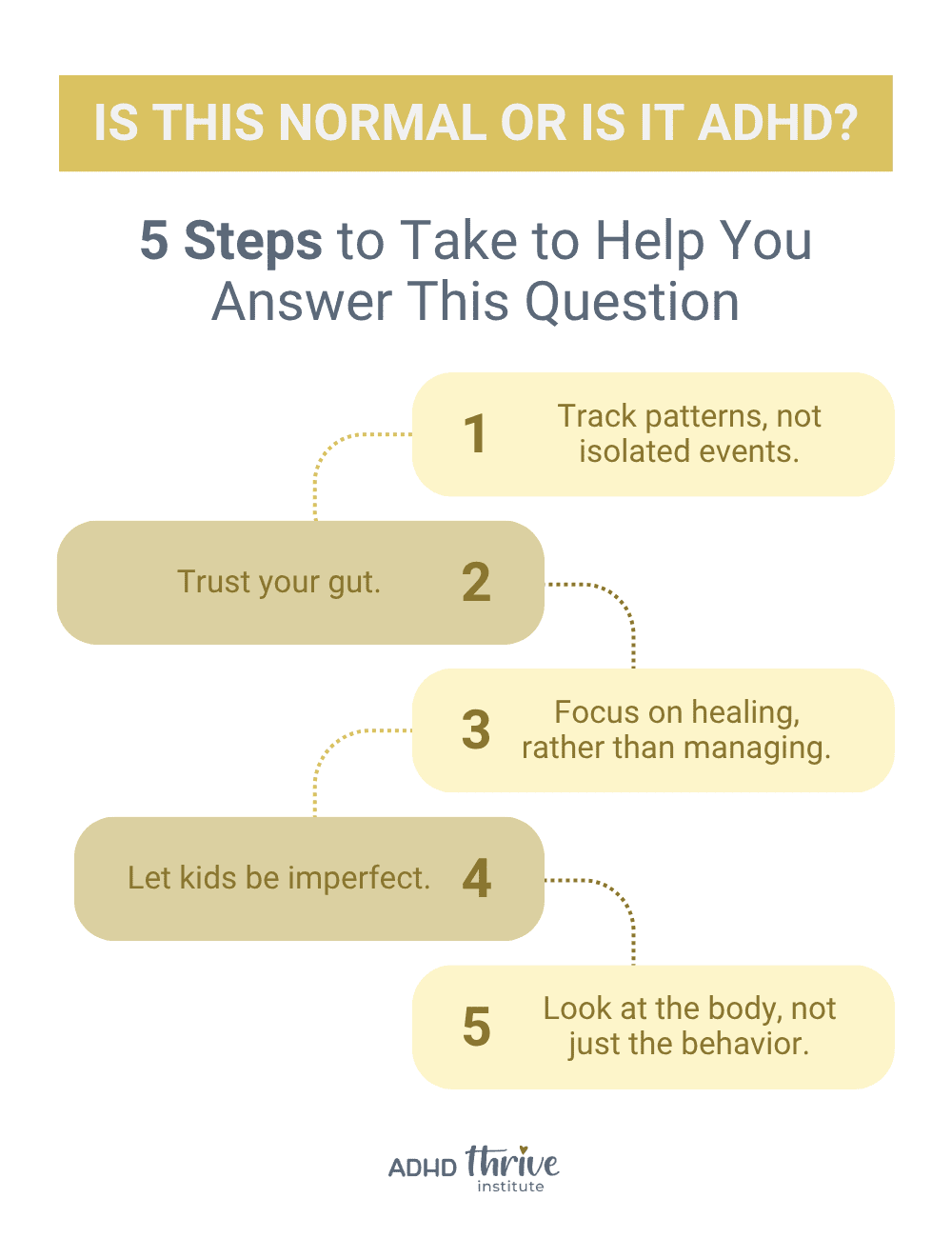
- Track patterns, not isolated events.
One bad day doesn’t mean something’s wrong. But consistent patterns of dysregulation, forgetfulness, or meltdowns over time can point to deeper issues. Pay attention to how often, how intense, and how disruptive certain behaviors are.
- Trust your gut.
You know your child better than anyone else. If your internal alarm bells are going off, even if others are brushing it off, remember that your observations matter.
- Focus on healing, rather than managing.
When we support the gut-brain connection, calm the nervous system, and reduce internal stressors, behavior shifts often follow.
Too often in traditional care, the focus is solely on managing symptoms. I believe there’s a better way.
In our ADHD Thrive Method 4 Kids program, we don’t focus on managing symptoms alone. Rather, we focus on healing the body from the inside out, so that those symptoms can begin to disappear on their own.
- Let kids be imperfect.
Remember, kids are still learning. Even neurotypical kids lie, meltdown over small things from time to time, and argue. They are still growing, and so are we. We are ALL allowed to have off days.
Perfection isn’t the goal. What’s important is understanding how age, development, and biology intersect.
Let’s take boys as an example. Normal kindergartner behavior in boys often includes rough play, high energy, climbing, noise-making, and sensory-seeking. Yet, these natural developmental traits are frequently labeled as “disruptive” or “problematic.”
Instead of pathologizing boyhood, we need to recognize that many of these behaviors reflect unmet sensory, emotional, or biological needs, not intentional defiance. Understanding how boys develop and how their brains and bodies process the world helps us respond with support, not punishment.
- Look at the body, not just the behavior.
Ask yourself this: 👉 “What is my child’s body trying to tell me?”
Because behavior is actually a messenger. It’s often not about willpower, defiance, or discipline. It’s about biology.
As I already mentioned, behavior is considered abnormal when it starts interfering with a child’s ability to function, thrive, and connect. But that doesn’t mean it’s just a brain issue. In many cases, it’s the body sending signals of distress.
So let’s shift the lens from labels to underlying stressors affecting biology.
Ask questions like:
- Is my child getting enough quality sleep?
- Could there be gut health imbalances at play?
- Are they eating foods that create inflammation or trigger their nervous system?
- Are nutrient deficiencies affecting their mood or focus?
If you’re ready to take that first step toward understanding what your child’s body might be trying to tell you, there are two easy ways to get started:
This resource breaks down the most common underlying stressors of ADHD symptoms and how to start addressing them naturally.
Many times, what looks like “ADHD” is really a symptom of internal stress, whether that’s poor detoxification, food sensitivities, low neurotransmitter support, or immune dysregulation.
When we address the biology underneath the behaviors, we can dramatically reduce symptoms and help kids feel better in their bodies and minds.
During this no-pressure call, we’ll talk about what you’re seeing in your child and whether functional lab testing might be the right next step. For many families, functional testing is a game-changer. It helps us uncover the underlying stressors behind symptoms.
Why the Fear Lingers (Even When Things Are Better)
Even when your child is doing better (having fewer meltdowns, more focus, and calmer days), many parents find that the emotional toll of the journey doesn’t disappear overnight.
I’ll never forget what one mom told me:
“When the phone stopped ringing, my nervous system didn’t know what to do. I had a panic attack—not because anything was wrong, but because for once, everything was right.”
That story hit me hard, because I’ve lived it too. There was a time in our journey when the school calls came so often that silence felt suspicious.
So when things started getting better, my nervous system didn’t know how to handle it. One meltdown would send me spiraling:
“Is this a setback?”
“Is the protocol still working?”
“What if we’re regressing?”
If you’ve ever found yourself in that fear loop—holding your breath, waiting for the next crisis—you are not alone. This is the reality so many parents of neurodivergent kids live in.
It takes time to heal from the stress of constantly being on alert.
We often talk about calming our kids’ nervous systems, but what about ours?
That PTSD-like punch in the gut when an old behavior reappears isn’t a sign you’re doing something wrong. It’s a sign that you care deeply. It’s a sign that you’ve worked so hard to create peace, and you’re scared of losing it.
That doesn’t make you weak. It means you’ve been living in survival mode for a long time, and healing takes time for parents too.
The Roller Coaster of Progress: What Healing Actually Looks Like
One of the biggest traps parents fall into on this journey is expecting healing to be a straight line.
It’s not.
Healing is messy. It’s nonlinear, and it often comes with ups and downs that feel like setbacks, even when they’re not.
Let’s say your child used to have six meltdowns a week… and now they’re having one. That’s huge progress. But here’s what often happens:
That one meltdown hits harder, because you’re no longer living in constant chaos. You’ve finally started to experience peace, so when something flares up again, it feels like a threat. Like maybe everything is unraveling. But it’s not.
This is where we have to ask better questions… not just “Is this a normal behavior?”
Better Questions to Ask Instead of, “Is this Normal?”
- “Is this still happening every day?”
- “Was the intensity the same as before or is it more manageable now?”
- “Did my child recover more quickly this time?”
- “Could this be tied to a known trigger… like poor sleep, a food reaction, or illness?”
Progress doesn’t mean zero symptoms. It means reduced frequency, lower intensity, and faster recovery.
This is especially important when we’re talking about normal behavior vs abnormal behavior.
Not every bad day means your child is backsliding. Sometimes they’re tired, hungry, stressed, or just being a normal human.
Even adults have off days, so why are we so quick to panic when our kids do?

Here’s the truth:
ADHD is real, ADHD is neurological, and ADHD isn’t something that’s simply “cured.” But that doesn’t mean change is impossible.
When we reduce the stress on the body — by supporting the gut, improving nutrient levels, and calming inflammation — we can support the brain in powerful ways. That’s what we focus on inside our programs.
So When Should You Take the Next Step?
If your child’s behavior is consistently disrupting daily life (at home, at school, in relationships), it’s time to dig deeper.
Because while some challenges are part of typical development, persistent struggles may be your child’s body signaling for help.
As mentioned, we have two resources to help: The Biology Beneath Behaviors Guide (which provides you with information on the most common underlying biological stressors driving symptoms) and the Free ADHD Thrive Breakthrough Call (where you can talk with our team about functional lab testing and how it can help uncover those stressors in the body).
You don’t have to navigate this alone. This is exactly what we help families with every single day.
So if you’ve been asking yourself “Is this behavior normal, or is it ADHD?”, remember: sometimes it’s both. Sometimes it’s a tired, growing child who needs more connection and better nutrition. Other times, it’s a flare-up of inflammation from a hidden trigger. Often, it’s a mix of biology, development, and environment all playing a role.
If you take one thing away from this post, let it be this:
Behavior is communication. It’s your child’s way of saying, “I need help,” even if they don’t have the words.
So whether your child is throwing shoes at the wall or refusing to eat breakfast because the strawberries “feel wrong”… pause before labeling it.
Get curious. Zoom out. Look for patterns. Maybe even journal what you’re seeing to gain clarity.
Because progress doesn’t always look like a straight line…but it always leaves clues.
And your child is still growing, still healing, and still becoming who they’re meant to be.
Let them be human. Let yourself be human too. You’ve got this. And I’ve got your back.
Frequently Asked Questions
- What is considered normal behavior in kids?
Normal behavior varies depending on a child’s age and development, but in general, it includes things like occasional forgetfulness, emotional outbursts during stress, and difficulty sitting still, especially in younger kids. These behaviors are part of typical brain development and don’t necessarily point to ADHD or any disorder.
- How do I know if my child’s behavior is abnormal?
Behavior may be considered abnormal when it is persistent, intense, and disrupts daily functioning at home, in school, or in relationships, despite support and structure. For example, daily meltdowns over small changes or an inability to follow basic instructions consistently could indicate something deeper is going on.
- What’s the difference between ADHD symptoms and normal behavior?
The difference often comes down to frequency, intensity, and impact. Occasional distractibility or hyperactivity is normal. But if these behaviors are constant and interfere with your child’s ability to function or thrive (despite strategies and accommodations), they may be signs of ADHD or an underlying biological stressor.
- Is ADHD real?
Yes, ADHD is a real, neurological condition supported by decades of research. However, it is often misunderstood, and symptoms can be influenced—or worsened—by internal factors like inflammation, nutrient deficiencies, gut imbalances, and food sensitivities.
- Is ADHD curable?
ADHD is not considered “curable” in the traditional medical sense, but symptoms can be significantly reduced when we address the underlying stressors in the body. Many families in our program have seen dramatic improvements in focus, emotional regulation, and behavior by supporting the gut-brain connection and calming internal inflammation.
- What age do ADHD symptoms start to show?
ADHD symptoms can start appearing as early as preschool, especially in high-demand or overstimulating environments. However, many children are not diagnosed until elementary school or adolescence, when academic and social demands increase. Symptoms may look different at different ages, and sometimes what’s considered “normal” in a kindergartner may be more concerning in a teen.
- Could my child’s behavior be something other than ADHD?
Yes. Many ADHD-like symptoms (such as hyperactivity, poor focus, or emotional outbursts) can be triggered by biological stressors like poor sleep, gut health issues, food sensitivities, or nutrient deficiencies. That’s why we encourage parents to look at the body, not just the behavior.
- When should I seek help?
If your child’s behavior is consistently interfering with learning, relationships, or daily routines, it’s time to dig deeper. You can start by tracking patterns, listening to your instincts, and considering functional testing to uncover hidden stressors that may be affecting their brain and body.
- What is functional lab testing and how can it help?
Functional lab testing goes beyond traditional blood work to uncover underlying stressors of symptoms, like food sensitivities, gut infections, nutrient depletion, and inflammation. It helps identify what’s really going on beneath the behavior so we can create a personalized support plan.
- What should I do if I’m still unsure?
You don’t need all the answers today. You just need the next step.
👉 Download our free guide: The Biology Beneath Behaviors
👉 Or book a Free ADHD Thrive Breakthrough Call to explore if functional testing is right for your child.
We guide families through this process every day, and we’d be honored to help you too.